In the year 2025, the prevention of pressure ulcers, commonly known as "Anti Decubitus" strategies, remains a critical focus within the healthcare sector. According to recent reports from the National Pressure Injury Advisory Panel (NPIAP), nearly 2.5 million patients suffer from pressure injuries annually in the United States alone, contributing to significant healthcare costs estimated to exceed $26 billion each year. The growing number of elderly individuals and those with limited mobility intensifies the need for effective prevention measures.
Adopting advanced techniques and innovative approaches can significantly reduce the incidence of Anti Decubitus injuries. Research suggests that implementing comprehensive risk assessment tools and regular monitoring can lead to a 60% reduction in such injuries amongst at-risk populations. Furthermore, a strong emphasis on staff education and training in proper repositioning techniques has been correlated with improved patient outcomes. As we progress into 2025, integrating technology and evidence-based practices will be pivotal in shaping the future landscape of Anti Decubitus care, ultimately ensuring better health and quality of life for vulnerable individuals.

As we look toward 2025, the landscape of anti-decubitus prevention is being revolutionized by emerging technologies that are set to transform patient care practices. One of the notable advancements is the integration of smart mattress systems equipped with pressure sensing and monitoring technologies. These mattresses can automatically adjust their firmness and position based on the patient's body weight and movements, significantly reducing the risk of pressure ulcers. Additionally, the ability to collect real-time data allows healthcare providers to track patients’ comfort levels and reposition them proactively.
Another promising area is the use of wearable devices that monitor skin health and detect early signs of pressure-related injuries. These devices can provide alerts to both caregivers and patients, enabling timely interventions. Furthermore, artificial intelligence (AI) plays a crucial role in analyzing patterns in patient data to predict the likelihood of decubitus formation, allowing for personalized care plans. As these technologies continue to evolve and converge, they hold the potential not only to enhance patient outcomes but also to streamline care delivery in healthcare settings, ensuring that anti-decubitus measures are both effective and efficient.
Innovative materials are at the forefront of strategies aimed at preventing anti-decubitus ulcers, a concern that is projected to affect millions of individuals, particularly those with limited mobility. According to a recent report by the National Pressure Injury Advisory Panel, an estimated 2.5 million patients develop pressure ulcers in the United States alone each year. As healthcare providers seek to improve patient outcomes, investing in advanced materials that promote pressure relief and comfort is becoming increasingly critical.
One innovative solution gaining traction is the use of dynamic support surfaces, which leverage advanced foam technologies designed to distribute weight more evenly across the body. These surfaces not only reduce localized pressure but also enhance comfort, encouraging longer periods of immobility without adverse effects. The pressure redistribution properties of these materials can decrease the incidence of ulcers by up to 50%, based on findings from recent clinical trials. Additionally, moisture-wicking fabrics integrated into the design help manage skin hydration, further mitigating the risk of tissue damage.
Moreover, we are witnessing the integration of smart materials that adapt to body changes, offering personalized support. Research indicates that temperature-regulating materials can enhance comfort by maintaining a stable thermal environment, thus supporting skin integrity. Reports suggest that when combining innovative materials with regular repositioning protocols, the overall efficacy of pressure ulcer prevention strategies improves significantly. This multifaceted approach highlights the importance of materials science in enhancing patient care and driving advancements in ulcer prevention strategies as we move towards 2025 and beyond.
| Strategy | Material | Pressure Relief (mmHg) | Comfort Level (1-10) | Durability (Years) |
|---|---|---|---|---|
| Smart Positioning | Memory Foam | 25 | 8 | 5 |
| Dynamic Cushioning | Gel-infused Materials | 20 | 9 | 4 |
| Adaptive Support | Viscoelastic Foam | 22 | 7 | 6 |
| Pressure Mapping | Air-Cell Systems | 18 | 8 | 3 |
| Routine Assessment | High-Density Foam | 21 | 6 | 7 |
In 2025, the prevention of anti decubitus ulcers hinges significantly on the advancement of personalized care plans and systematic risk assessment strategies. Recent studies indicate that about 2.5 million patients in the United States develop pressure ulcers each year, leading to substantial healthcare costs and increased morbidity. Personalized care plans that address individual patient profiles—such as mobility, nutritional status, and skin condition—are essential in reducing this incidence. By tailoring interventions, healthcare professionals can better target high-risk individuals and implement preventive measures effectively.
Risk assessment is further enhanced by incorporating evidence-based tools such as the Braden Scale, which evaluates factors like sensory perception and moisture level to predict ulcer formation risk. Current data suggest that consistent use of such assessment strategies can decrease the prevalence of pressure ulcers by up to 30%. In addition to using established assessment scales, integrating technology such as electronic health records can facilitate real-time monitoring and adjustments to care plans. Engaging in proactive risk assessment ensures that caregivers can identify at-risk patients early and implement necessary interventions to mitigate the risk of developing decubitus ulcers, ultimately leading to improved patient outcomes.
Training healthcare professionals on best practices for preventing anti-decubitus is imperative in the modern healthcare landscape. As bedsores, also known as pressure ulcers, continue to impact patient outcomes significantly, equipping medical staff with the necessary skills and knowledge is crucial. Comprehensive training programs should focus on the identification of at-risk patients, the implementation of frequent repositioning schedules, and the utilization of specialized equipment designed for pressure relief.
Incorporating evidence-based practices into ongoing education can empower healthcare professionals to make informed decisions about patient care. Workshops and certification courses can provide hands-on experience with innovative techniques, such as advanced wound assessment and the application of modern dressings that promote healing. By fostering an environment of continuous learning, healthcare facilities can ensure that their staff remains knowledgeable about the latest protocols and technologies, ultimately improving patient safety and comfort. Regular evaluations and updates to training modules will also help maintain high standards and adapt to new challenges in patient care.
This chart illustrates the effectiveness of various strategies for preventing anti decubitus ulcers in healthcare settings, based on best practices and training for healthcare professionals. The data represents the percentage increase in effectiveness of each strategy from 2020 to 2025.
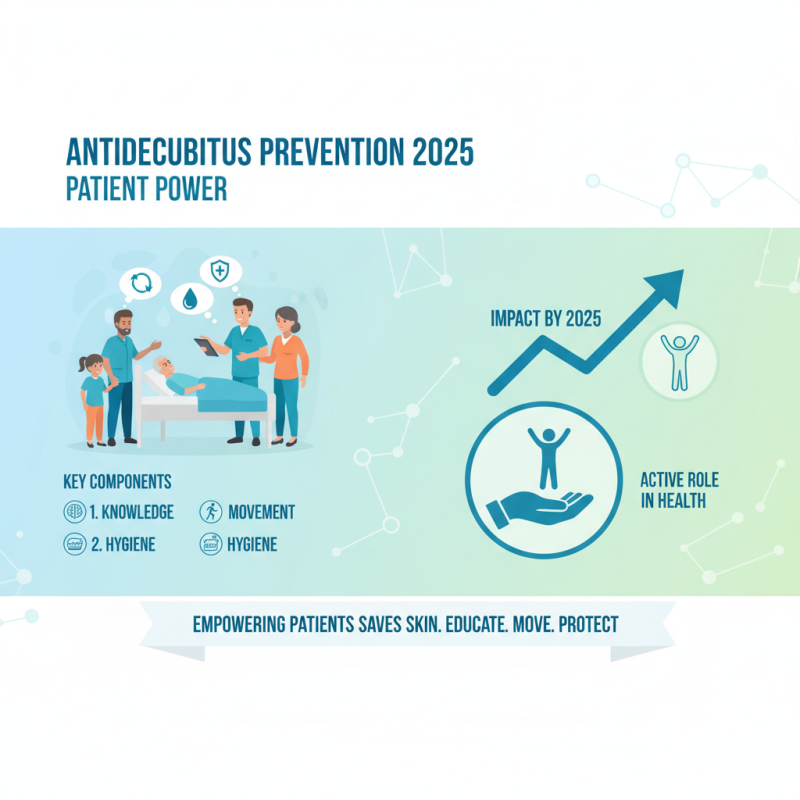
Patient education and engagement are critical components in the effective implementation of strategies designed to prevent anti decubitus, particularly as we look ahead to 2025. Empowering patients with knowledge about their conditions and the importance of regular movement is essential. By understanding the risks associated with pressure ulcers and the factors that contribute to their development, patients can take an active role in their own healthcare. Simple education sessions can be conducted during hospital stays, focusing on the significance of proper body positioning, the need for frequent changes in position, and the importance of maintaining skin hygiene.
Additionally, fostering patient engagement through interactive approaches, such as workshops and personalized care plans, can enhance motivation and adherence to preventive measures. Tools like mobile apps or online portals can provide patients with reminders for mobility and daily skin checks, ensuring they remain informed and accountable. Collaboration between healthcare providers and patients is vital; by encouraging patients to voice their concerns and preferences regarding their care, we can create a more tailored and effective approach to preventing anti decubitus. This partnership not only improves outcomes but also enhances the overall patient experience in their journey towards better health.